Informed choice isn’t just for residents. Choose the right language. Part 2 of a four-part blog series
Gail Douglas: In a past article we heard from culture change advocate Carmen Bowman about how person-centered care is changing the language we use — from institutionalized to normal words — and how the new CMS rules address this issue. Now I’d like to ask your thoughts about the changes in the language as they apply specifically to dining services.
Diane Hall: This is something that I’ve been pushing for years and it’s finally happening. When you read the new requirements with the changes highlighted in red it becomes readily apparent that the language is now focused on the resident and their right to make informed choices about what, when and where they eat. And complying with those person-centered mandates is tied to the five-star rating system that leads people to your community.
GD: I know you just got back from a well-deserved invitation to speak, along with Bill Lutz from Optimum Health, at the 2017 National Pioneer Network’s conference. What issues did you address in your presentation that dealt with the language of informed choice?
DH: I touched on the differences between the new dining standards and the reformed federal regulations, the core components of the performance improvement program and implementing self-directed dining through the care plan process. I wanted to show how the reformed regulations are now in alignment with new long-term care dining practices.
GD: How so?
DH: The language of the reformed CMS regulations is all about the individual, which reflects the language in the dining standards about individualizing nutrition approaches, diet liberalization and honoring choice. So, the focus is on supporting self-directed living and not traditional professional or family control.
GD: Can you give us an example of how the language has changed in the Final Rule?
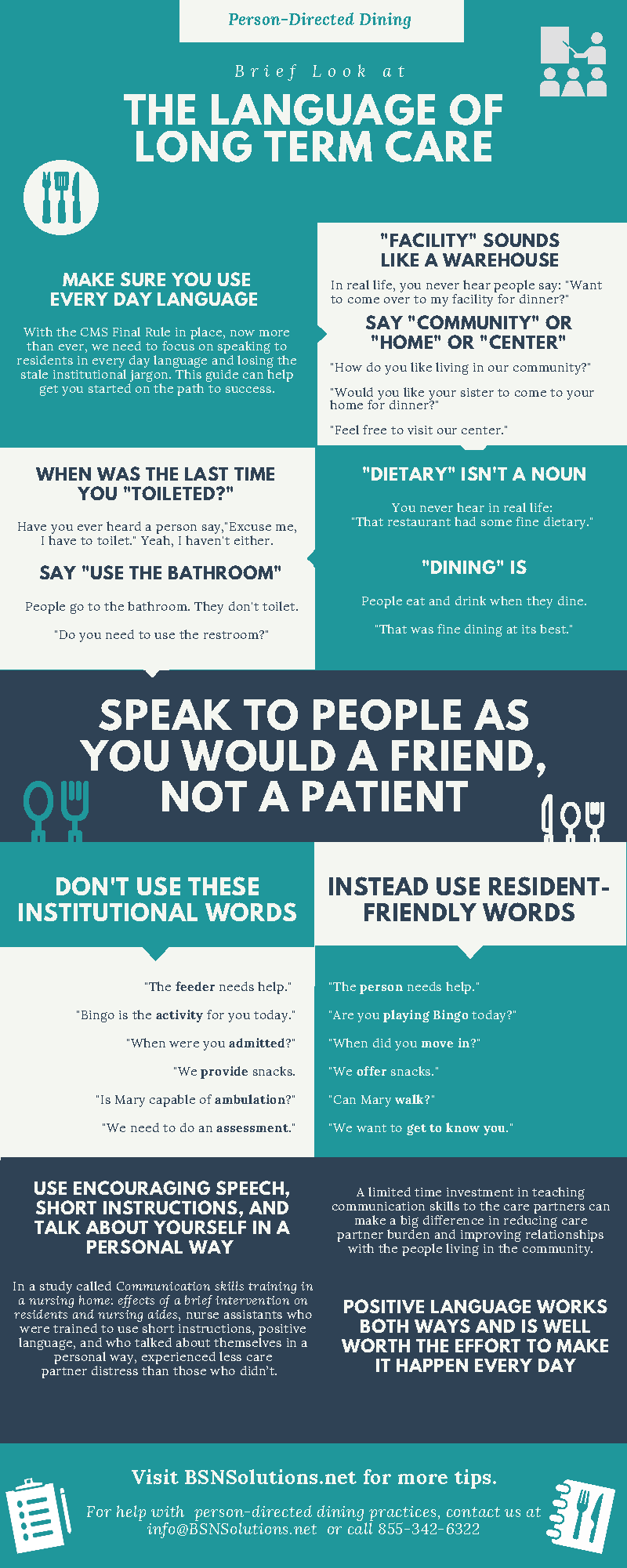
DH: One big change is centered on making sure that the resident understands his or her rights by speaking in a language that can be understood. I did a search on the word “language” in the CMS Interpretive guidelines and saw over and over again variations of the requirement to use “language that he or she, they, or the resident understands.” That means speaking in plain English and not healthcare jargon.
GD: That is definitely a big change away from institutionalized practices.
DH: I read a quote from Denise Hyde, Community Builder at The Eden Alternative, about focusing on positive language by emphasizing a resident’s choices rather than their noncompliance and focusing on a person’s strengths and not their weaknesses. She’s right. The way we say things can be so powerful and can set the tone for creating productive dining plans that satisfy residents while keeping them as safe as possible.
GD: It’s just another example of putting the resident first.
DH: Yes, but we could be forgetting something equally important when we focus solely on the resident.
GD: What’s that?
DH: Well, when I started thinking about the effects of positive language on nursing home care, I searched “positive language and nursing home care” to see what was out there on the internet. I found an interesting study published in Clinical Interventions in Aging 1 about teaching nurse assistants communication skills like positive speech, using short instructions, and biographical statements when talking to residents. It was a small study, but the interesting thing about it was that not only did it look at the effect of positive language on residents, but also how using positive communication skills affected the nurse assistants.
GD: And what did the study find out about teaching communication skills to nursing staff?
DH: Positive language works both ways. After training, nurse assistants who were trained to use short instructions, positive language, and who talked about themselves in a personal way, experienced less caregiver distress than those who didn’t. While as I said this was a small study, it did show that even a limited time investment in teaching communication skills to the staff can make a big difference in reducing caregiver burden and improving relationships with the people living in the community.
GD: So, using plain English and positive language can benefit both the people living and working in a community?
DH: Exactly. Plain English and positive language is one of things we focused on when we were coming up with our documentation tools for creating dining plans that address diet restrictions. We created tip sheets and risks and benefits for each of the big six diet restrictions (for example,fluid restrictions). Each one is written in plain language so care providers can easily explain the information to residents.
GD: Is that why the Inside Scoop on Informed Choice manual was written like a movie script with characters representing real people in conversation?
DH: Yes. We found to be a very effective way to communicate and show how to speak to residents using plain language in a way they would understand. And it’s absolutely essential that residents fully understand and accept the risks they may be taking when liberalizing their diet.
GD: Speaking of care plans, that’s the subject of our next installment about using plain language when creating care plans that residents and their advocates understand.
DH: I’m looking forward to it.