Pioneer Village resident Mary H. had one big concern about her diet. She didn’t want to be given a diet plan based solely on the fact that she has a diagnosis of diabetes. At the nursing home she had just left, the attending physician prescribed a diabetic diet without even talking to her about it. That kind of diagnosis-based diet comes from the institutionalized thinking that doctors and nursing home staff should be trying to get away from, especially if they want to stay bulletproof in the citation department. The CMS regulations make it clear that Mary H. has the right to informed choice and can refuse the prescribed diet. Every professional caring for Mary H is obligated to honor her wishes and prescribe her diet of choice. Here’s where documentation through the care plan process becomes REALLY important.
Regulation: CMS F325 483.25(i) Nutritional Status
“A resident or resident’s representative has the right to make informed choices about accepting or declining care and treatment. The facility can help the resident exercise those rights effectively by discussing with the resident (or the resident’s representative) the resident’s condition, treatment options (including related risks and benefits, and expected outcomes), personal preferences, and any potential consequences of accepting or refusing treatment. If the resident declines specific interventions, the facility must address the resident’s concerns and offer relevant alternatives.”
Dietary Goals for Mary H
Mary H. had dealt with diabetes for years, and had always managed her blood glucose levels well on her own. She wanted to stay in control of what and when she ate. She wants to eat a regular diet, and be offered regular and healthful desserts and snacks. She wants to be able to eat snacks when and where she wanted. She will be happy to inform the nurse when she has consumed more carbohydrates than usual.
Current thinking and research on Diabetic Diet
“There is no evidence to support prescribing diet such as no-concentrated sweets or no-sugar added for older adults in living in healthcare communities, and these restricted diets are no longer considered appropriate. Most experts agree that using medication rather than dietary changes to control blood glucose, blood lipid levels, and blood pressure can enhance the joy of eating and reduce the risk of malnutrition in older adults and healthcare communities.” — Academy of Nutrition & Dietetics
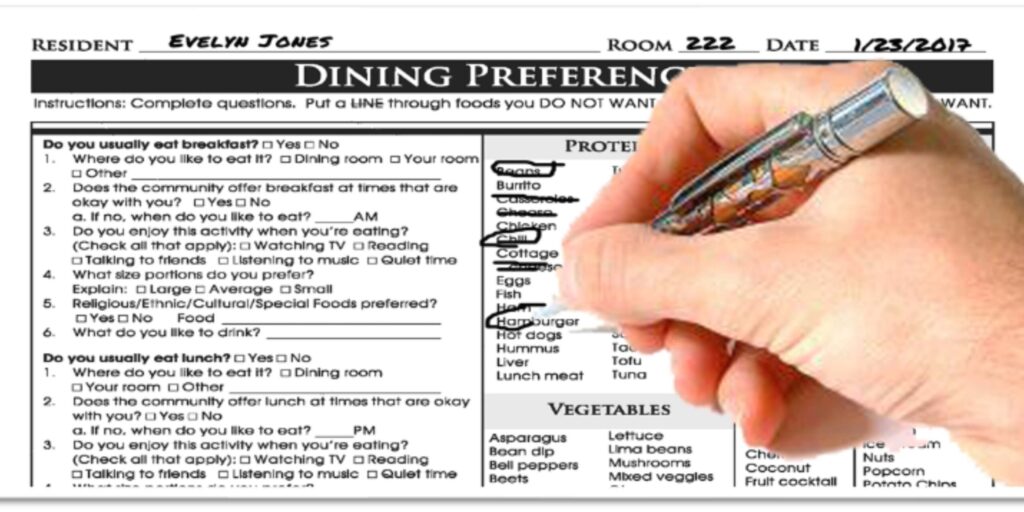
The resident directed care planning process
Mary H met with the care plan team at Pioneer Village, and together they developed a plan of care that documents her informed choice about her diet and goals. If her decision goes against what the clinical team recommends, the care plan provides written proof of that the risks, benefits and alternatives of the diet plan have been discussed with Mary H. Mary H felt that she made her wishes known and her decisions were honored, and the care plan process provided collaboration between her allowed her to collaborate with her caregivers to develop a plan that truly balances quality of life with quality of care