Part Four – How to Increase Referrals – and Income – Using Person-Directed Dining
This is the final part of our interview with Diane Hall about the 5 Star Quality Ratings System and its impact on skilled nursing homes.
So, Diane, in the last blog we talked about losing referrals for having a below average 5-Star Quality Rating and how it can affect a home’s bottom line. Now let’s take off your administrator hat and put on your registered dietitian cap and talk about some of the things that a nursing home can do from a nutritional standpoint to help the community score well in the 5-Star Rating System.
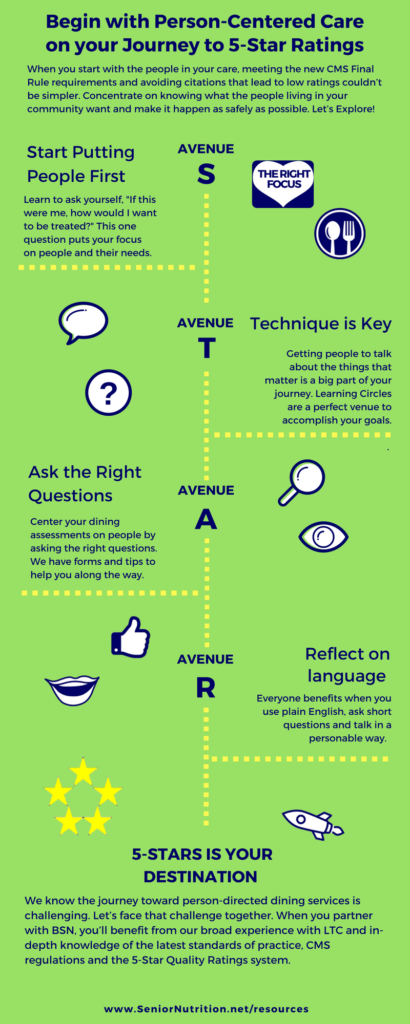
It all starts with rolling out a person directed dining initiative, which means developing a relationship with the person living in your community. That’s the key that opens the door to everything else.
If you don’t put the focus on your residents and their right to have choices about what, when and where they eat, you are putting yourself behind the eight ball when it comes to getting above average ratings
In your opinion, what is the most important component for making person-directed dining happen in a community?
It has to be the dining care plan. Everything related to a person’s choices about his or her diet stems from this written plan. Written information and documentation tools to provide residents with what they need to make informed decisions about their meals, drinks and snacks are critical. If a resident chooses to or not to accept diet restrictions, someone must discuss and document the risks, benefits and options about the diet. That’s why we created a manual with tons of resources and forms that help communities safely honor a person’s choice while staying in compliance with new, mandated requirements from CMS.
So what you’re saying is that it all starts with a clear understanding of the resident’s diet goals. It is the job of the care plan team to create approaches to ensure the person’s goals are attainable and the risks are well managed. And of course, we have to monitor any unique approaches that have been developed to honor dining goals.
Yes. I wanted to create something so communities didn’t have to reinvent the wheel. To do this, there is a form in the manual that guides people through the documentation process of the discussion about the risks and benefits of diet choices. We chose the five most common diet restrictions in long term care; Diabetic, Cardiac, Altered Consistency, Fluid Restriction and Tube Feeding. That way communities can use this information to fill out the person’s existing care plan forms but still customize to his or her unique condition.
Once they have a process in place for creating dining care plans, what else do they need to do to kick up their ratings?
As we talked about in the last blog, identifying and reducing the number of deficiencies and the severity of problems, is a major part of the health inspection component of the rating system.
Right. If I remember correctly, it accounts for over half of your score.
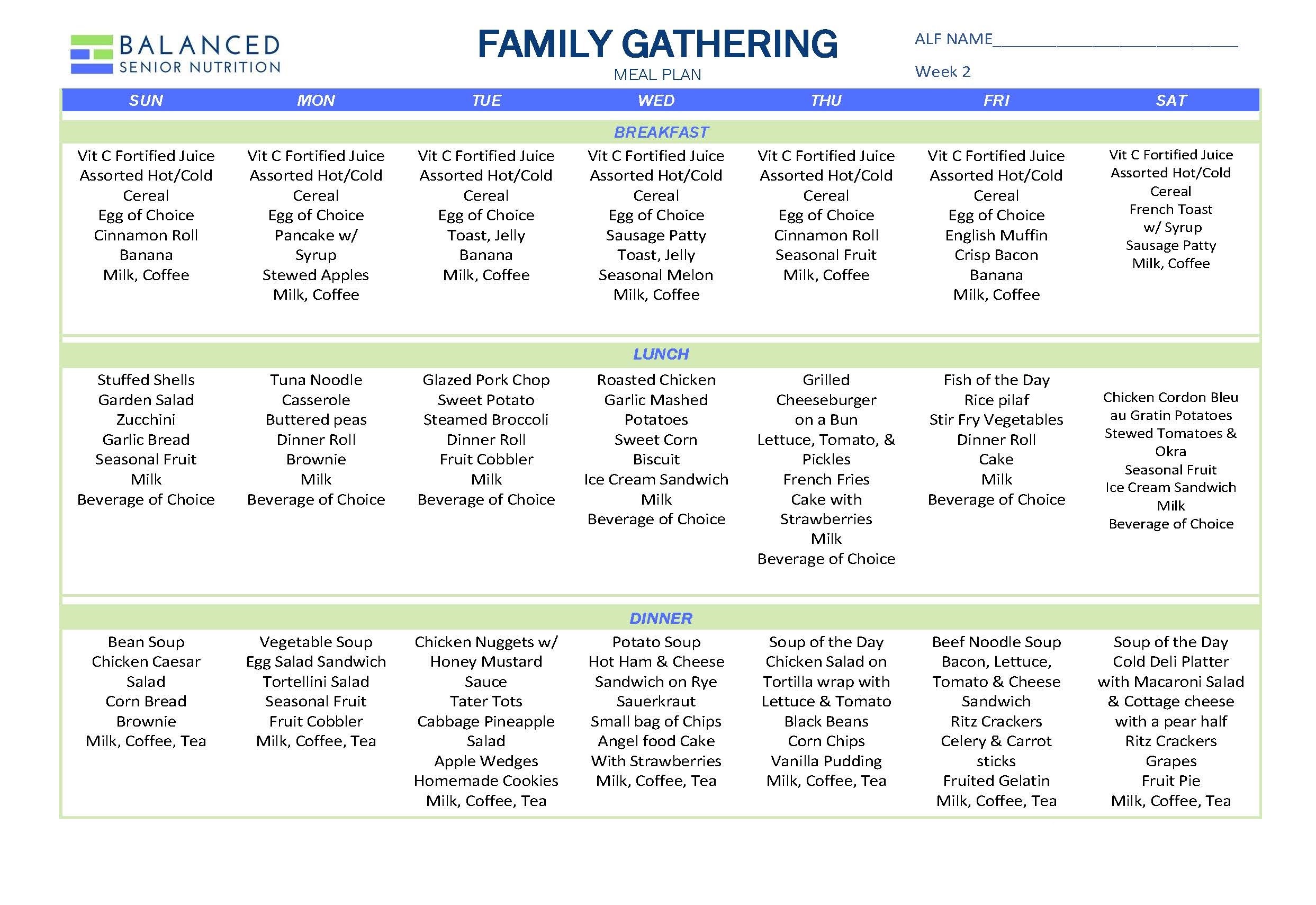
That’s right. From a nutrition standpoint, that means serving people appealing food and drink they want, and at the temperature they want. (You know, hot foods hot and cold foods cold for most folks.) That means having snacks available for people when they want them just like they had snacks available at home. It also means knowing the person well enough to quickly realize when his or her feeding skills decline or food and drink intakes change. In short, you must constantly assess dining services and survey residents to make sure that mandated requirements are being met.
How does that relate to the five-star quality rating system?
A great deal of the rating is based on having accurate documentation to show where problems existed and how they’ve been corrected. Communities must have developed Quality Assurance Performance Improvement (QAPI) processes that ensure compliance to regulations, especially those related to person-centered care. That’s why we developed survey and assessment forms related to dining requirements and dining satisfaction that can be used to find out where opportunities for improvement exist. Now, you can quickly start the process of creating action plans and projects to close those gaps in performance.
Once you identify an opportunity for improvement using a resident dining satisfaction survey, what happens next?
learning circle info promo
We suggest forming a learning circle composed of the people — and I’m including both staff and residents — most affected by the issue so they can discuss what may be the root of the problem. That way, a task force can come up with a plan to close any gaps in performance. This problem-solving process is part of the CMS mandated requirement (F865) for a QAPI program.