Gail Douglas: In this series, I will be interviewing Diane Hall, president of BSN Solutions, author of The Inside Scoop on Informed Choice, former administrator and a long-time advocate for person-directed dining practices. Diane has a unique perspective on the requirements in the new Final Rule from the Centers for Medicare and Medicaid Services and how those requirements will affect the Five-Star Quality Rating System with regard to person-centered care.
GD: Diane, a lot has changed in the final CMS rule guidelines regarding person-centered care. From a dining point of view, what is the big takeaway from these changes and how do they relate to the 5-star rating system?
DH: I think the big takeaway is the shift in focus to what matters most to people living in LTC communities and away from institutionalized thinking that focuses on what’s easiest for the staff. In fact, if communities simply focus on creating dining care plans that provide people with choices of meals and snacks that they want, they will go a long way towards meeting the final rule guidelines and avoiding citations. By putting the resident front and center in the discussion of what matters to them most and how to safely achieve that goal, compliance with the new requirements will follow naturally. CMS believes this also. That is why the CMS Requirements of Participation, State Operation Manual (SOM), includes the definition of Person-centered care in the Appendix PP:
“Person-centered care means the facility focuses on the resident as the center of control, and supports each resident in making his or her own choices. Person-centered care includes making an effort to understand what each resident is communicating, verbally and nonverbally, identifying what is important to each resident with regard to daily routines and preferred activities, and having an understanding of the resident’s life before coming to reside in the nursing home. And we all know, compliance to requirements lead to higher ratings on the five-star rating system.”
GD: What is an effective step to communicate that change in focus to residents?
DH: Information written in plain language that people can understand. First and foremost, you must inform the resident that they have a choice. We use a handout that we give to new residents called the Declaration of Dining Independence. It says that residents have the right to make an informed choice and explains what a person can expect during their dining care plan meeting.
GD: By using this document, you are informing the resident of his or her dining rights, which meets the federal mandate that the person must be told about their rights. Is that correct?
DH: Exactly. The next thing to do when putting the resident front and center is to provide the opportunity to make personal choices based on what matters to that person.
GD: Are you taking about food choices?
DH: Not just food choices, but portion size and where they want to dine, as well. By concentrating on the many aspects of dining preferences, we get a comprehensive guide to the choices that will help in developing the plan of care. Another new CMS requirement I should mention is that of obtaining religious, cultural, and ethnic food preferences. Again, CMS shows support for person-centered dining.
GD: Once you have this comprehensive list of preferences, what’s the next step in the shared decision-making process?
DH: The care team and the resident discuss the details of what is uniquely important to the resident.
GD: Details such as?
DH: Explaining the risks and benefits of food choices and how those risks may adversely affect the resident and – this is key – to support the decision made by the resident, even when others may consider it risky. To do this, the care team must develop approaches to manage the risks and desires as safely as possible.
GD: Can you give us an example?
DH: Sure. We have tip sheets that highlight the risks and benefits of diet restrictions as well as the risks and benefits of liberalizing those diets. After discussing each of these, we can then explore the approaches for making potentially risky diet decisions as safe as possible.
GD: Does the risk and benefits tip sheet have a place to records a resident’s concerns about changes to their diet and the approaches to address those changes safely?
DH: No. We have a comprehensive form called Informed Choice Made Easy that covers those bases about what’s important to a person and what’s not in providing the evidence-based information regarding diet liberalization. It also lists approaches to diet liberalization to trigger the discussion about how best to accommodate a person’s preferences as safely as possible. The form also makes sure to document that the person understands and accepts the risks and benefits of their informed choice with regard to their dining preferences.
GD: Can you put on your administrator’s hat for a moment and let’s talk about how this model of the shared decision-making process can affect your bottom line?
DH: As we’ve discussed before, the surge of baby boomers has begun, and these folks have different expectations. They are not going to accept communities that don’t meet their standards. So, where are they going to go to start their search for places they may want to live? In my mind, the first place they’ll go is the government website that shows a rating of nursing homes near the location they choose. (www.Nursing Home Compare.gov)
GD: That’s logical since it breaks down the ratings into the three weighted categories: annual health inspections, staffing and quality measures. There is a magical formula that uses all this data to come up with the overall 5-star quality rating.
DH: Right. I should note that the outcomes of the health inspections account for over half of the overall rating so compliance to CMS requirements is incredibly important. The health inspections include the number (“scope”) and severity of deficiencies, and what actions were taken to correct deficiencies and/or complaints. CMS gives greater weight to deficiencies that cause “immediate jeopardy to resident health or safety” when determining each nursing home’s score, particularly when the infractions are widespread (affecting many people) and not just isolated incidents (affecting few people).
GD: So, it’s important that deficiencies are corrected after the first visit?
DH: Absolutely. If the deficiencies are still there on re-visits, you will lose those precious stars you worked so hard to get.
GD: Sounds like you need assessments and surveys that accurately record problems, investigate those complaints and gaps of performance, and create improvement projects to correct those deficiencies.
DH: And these surveys must be based on satisfying the people living in the community because that is what the new CMS requirements mandate. Again, we see that by shifting the focus on the resident as the locus of control over his or her own daily life, compliance to the final CMS rules improve and five-star ratings increase. And let’s not forget, that receiving less than a three-star rating can have dramatic effects on your community’s ability to get referrals from hospitals. So, focus, focus, focus on providing and honoring individual choices.
GD: Supporting people to provide the things that matter most builds healthy relationships and recognizes that there is an interdependence on each other to make a sometimes-difficult situation more tolerable.
DH: Let’s not forget that working with people in long-term care communities can be challenging, frustrating and rewarding – all in the same day. We just have to remember that the people we care for once cared for themselves and it is a tough adjustment to make when you have to turn certain aspects of your life over to others.
GD: That’s good advice and I’m looking forward to our conversation next week.
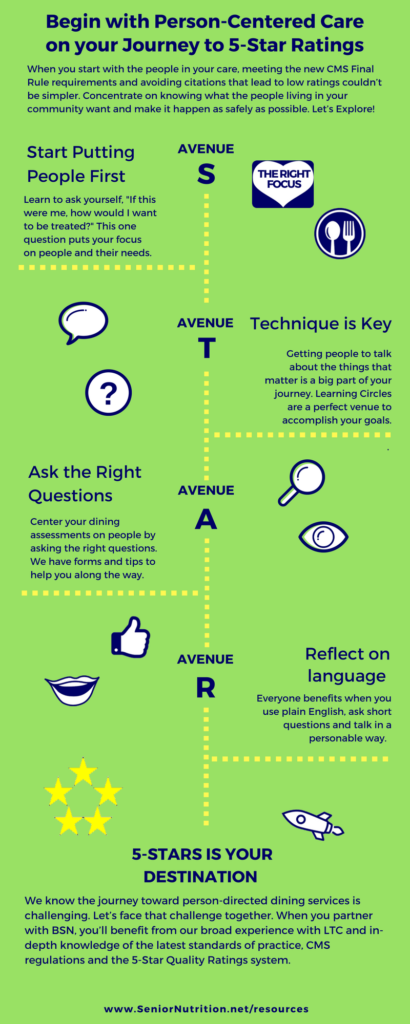
Giveaway. Infographic.










