Do Your Care Plans Accommodate Person-Directed Dining?
Making self-directed dining happen in our communities is up to us, the people working in them. To take communities, step-by-step, through this process we have created a manual, The Inside Scoop on Informed Choice.
In past blogs, we’ve talked about 13 institutional words or phrases you should stop using to change to a more person-centered mindset. We spoke of how changing to a self-directed dining plan makes good business sense. We even discussed the proper terms to use when changing to a culture that offers an informed choice to people. We know when a physician orders a restricted diet, an informed consent must be obtained from the resident to show his or her acceptance or refusal of the diet order. We also are aware that a care plan meeting needs to be scheduled that includes adequate information so a reasonable decision can be made. After the discussion, a plan needs to be written about what matters most to the individual while keeping him or her as safe as possible.
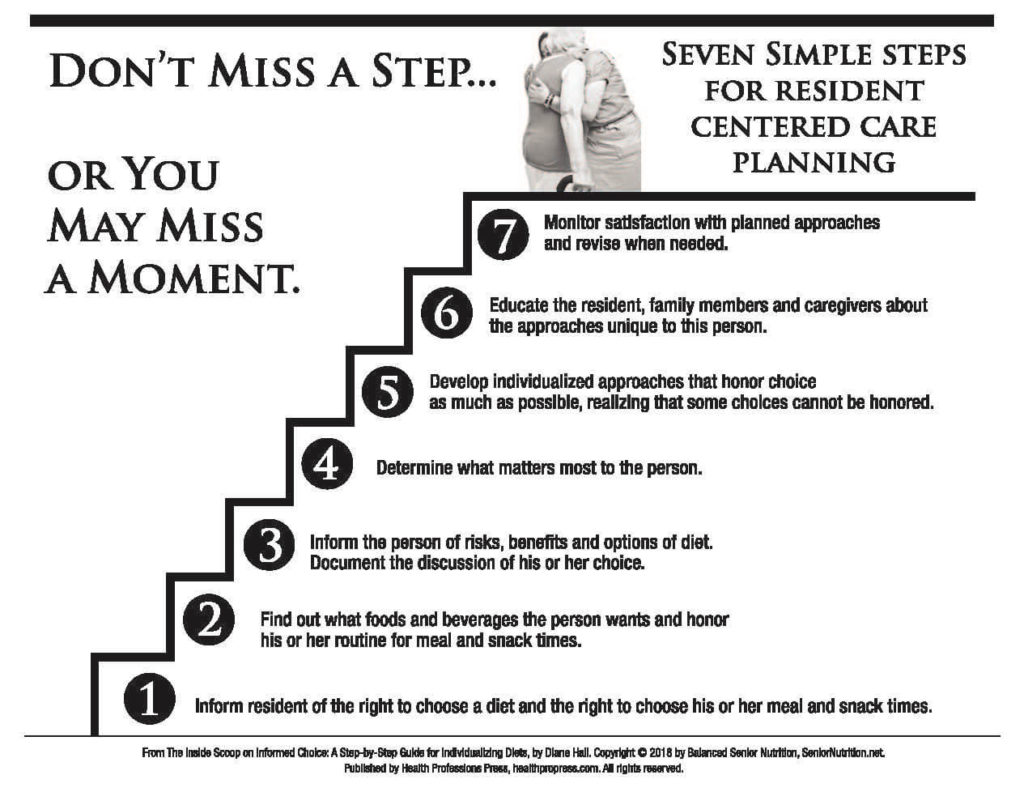
I would like to share with you seven simple steps, outlined in the manual, that will help you create a comprehensive self-directed dining care plan based on a resident’s right to make an informed choice about what, when and how they eat.
Step One: Who Should Be There?
The following people will assist the resident and/or surrogate in developing a written record of what matters most to him or her:
- Family members invited by the resident
- His or her physician. (If he or she cannot physically attend the meeting, suggest the doctor call in.)
- Care partner
- Licensed nurse
- Dining manager
- Social worker
- Any other appropriate health professionals
Step Two: How Will You and the Resident Know What You Discussed?
At the meeting, give the resident a copy of a document that lists the risks and benefits for his or her prescribed diet. Use it as a guide to discuss all of the associated aspects of the diet restriction. Check off each relevant point and add individualized comments about the resident’s concerns, questions and comments for preferences. As evidence of this discussion, we suggest written quotes, audio or video recording. (You don’t need to reinvent these documents. We developed Risk and Benefit tip sheets for the five major restricted diets, included in The Inside Scoop on Informed Choice).
Step Three: Where Will You Document What Is Discussed?
A documentation tool helps to validate that an informed choice has been made after options and consequences were discussed with the resident and written information was given to him or her. (The Informed Choice Made Easy tool is the centerpiece of our manual)
Step Four: How Will You Validate the Resident’s Informed Choice?
Request that the person sign the documentation tool as a record of his or her informed consent of diet. Request all the people in attendance also sign the document. The team uses this information to write the care plan.
Step Five: How Will You Honor a Resident’s Dining Choices?
To honor dining choices, follow through on any actions the team needs to take to support and sustain the individualized approaches chosen. Document in the progress notes as needed. Update a Dining Preference form (click to download our version for free) during the meeting process and update as needed.
Step Six: How Will You Monitor and Assess the Plan of Care?
At least quarterly, and as needed, inform and educate the resident again about his or her diet decisions. Review with the resident the outcome of the planned approaches and document his or her acceptance of the current plan of care.
Step Seven: How Will You Monitor and Assess YOUR Performance?
As part of Quality Assurance Performance Improvement (QAPI) initiative, review actions taken to accommodate individualized dining choices of the people in the community. Identify opportunities and use Performance Improvement Projects (PIP) when your systems are falling short of meeting the needs and requests of the people you are serving (the QAPI approach is discussed in The Inside Scoop on Informed Choice).
More importantly, you will be providing residents with meaningful meals that will keep them happy, healthy and as safe as possible.











21 Responses to Seven Steps to Creating a Dining Care Plan for Restricted Diets in Long Term Care